In recent years, the United States has witnessed an alarming resurgence in syphilis cases, reaching levels not observed since 1950. This trend has sparked widespread concern among healthcare professionals, policymakers, and public health experts due to its significant implications for public health.
The resurgence of syphilis represents a complex and multifaceted challenge, posing severe threats to individual health and community well-being. As such, addressing the syphilis epidemic has become a top priority for public health authorities nationwide.
This article aims to provide an in-depth analysis of the current syphilis epidemic in the United States, exploring its causes, impacts, and potential solutions. Key topics to be covered include the epidemiology of syphilis, factors contributing to its resurgence, public health response and interventions, and the broader implications for healthcare systems and communities.
By shedding light on the alarming rise in syphilis cases and examining its far-reaching consequences, this article seeks to raise awareness, prompt action, and facilitate informed discourse on this pressing public health issue.
Read more: Battle Against Shame for People Living with HIV in the U.K.
Understanding Syphilis
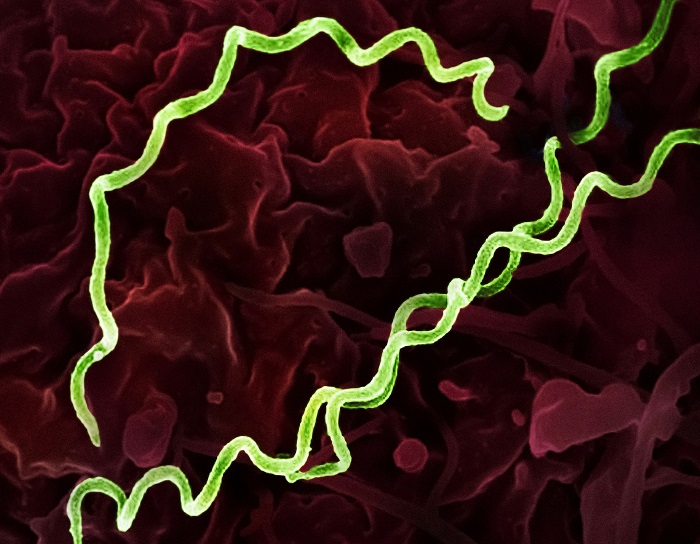
Syphilis, a sexually transmitted infection (STI) caused by the bacterium Treponema pallidum, is characterized by its diverse manifestations and stages. Initially, syphilis presents with painless sores, known as chancres, at the site of infection. If left untreated, the disease progresses through multiple stages, including secondary syphilis, characterized by skin rashes and mucous membrane lesions, and tertiary syphilis, which can lead to severe complications such as neurosyphilis, cardiovascular syphilis, and gummatous lesions.
Syphilis is primarily transmitted through sexual contact, including vaginal, anal, and oral sex, as well as through vertical transmission from mother to child during pregnancy or childbirth. Additionally, syphilis can be transmitted through blood transfusions or direct contact with syphilitic sores, although these modes of transmission are less common.
The historical context of syphilis in the United States traces back centuries, with notable outbreaks and epidemics documented throughout history. The introduction of penicillin in the mid-20th century led to a significant decline in syphilis rates, culminating in its near-eradication by the 1950s. However, in recent decades, the United States has experienced a resurgence of syphilis cases, with rates reaching levels not seen since the mid-20th century.
Several factors contribute to the resurgence of syphilis cases in the United States. Changes in sexual behaviour, including an increase in high-risk sexual practices such as unprotected sex and multiple sexual partners, have played a role in facilitating syphilis transmission. Additionally, disparities in access to healthcare, socioeconomic factors, and stigma surrounding STIs have hindered efforts to control the spread of syphilis.
The resurgence of syphilis represents a significant public health challenge, requiring coordinated efforts from healthcare providers, policymakers, and community stakeholders to address. By understanding the causes and consequences of the syphilis epidemic, stakeholders can develop targeted interventions and strategies to reduce transmission rates and improve health outcomes for affected individuals.
Epidemiology of Syphilis in the U.S.
Analysis of recent epidemiological data reveals a concerning trend of increasing syphilis cases in the United States. According to the Centers for Disease Control and Prevention (CDC), reported cases of syphilis have been on the rise in recent years, with significant implications for public health.
Demographic trends in syphilis cases indicate disparities in infection rates across different population groups. While syphilis affects individuals of all ages, races, and socioeconomic backgrounds, certain demographic groups are disproportionately affected. Young adults, particularly those aged 20 to 29 years, have been identified as a high-risk population for syphilis transmission. Additionally, men who have sex with men (MSM) and individuals living in urban areas are at increased risk of syphilis infection.
The geographic distribution of syphilis cases in the United States varies, with higher incidence rates observed in certain regions. Urban centres, including major metropolitan areas, tend to have higher concentrations of syphilis cases compared to rural areas. However, syphilis transmission can occur in any community, and efforts to address the epidemic must be tailored to local contexts and needs.
Comparing current syphilis rates with historical data highlights the resurgence of the infection in the United States. While syphilis was nearly eradicated by the mid-20th century, recent decades have seen a reversal of this trend, with rates reaching levels not seen since the 1950s. This resurgence mirrors global trends, as syphilis remains a significant public health concern worldwide.
Addressing the epidemiology of syphilis in the United States requires comprehensive surveillance, prevention, and intervention efforts. By analyzing recent data and identifying demographic trends, healthcare providers and policymakers can develop targeted strategies to reduce syphilis transmission rates and improve health outcomes for affected individuals. Additionally, increased awareness, education, and access to testing and treatment are essential components of efforts to combat the syphilis epidemic and protect public health.
Factors Contributing to the Syphilis Epidemic
The surge in syphilis cases in the United States can be attributed to a combination of factors that contribute to its spread and persistence. Understanding these factors is crucial for developing effective strategies to combat the syphilis epidemic.
Changes in sexual behaviour play a significant role in driving the surge in syphilis cases. Factors such as an increase in high-risk sexual practices, including unprotected sex and engaging in sexual activity with multiple partners, contribute to the transmission of syphilis. The rise of social media and dating apps has also facilitated connections between individuals, including those engaging in high-risk behaviours, leading to increased transmission rates.
Healthcare access disparities exacerbate the syphilis epidemic, particularly among marginalized and underserved populations. Limited access to healthcare services, including sexual health education, screening, and treatment, disproportionately affects individuals from low-income communities, racial and ethnic minorities, and LGBTQ+ populations. These disparities contribute to higher rates of undiagnosed and untreated syphilis infections, perpetuating the epidemic.
Read more: A History of Herpes in the Age of Making Out.
Challenges in STD prevention and treatment also contribute to the syphilis epidemic. Despite advancements in medical technology and treatment options, barriers such as stigma, discrimination, and lack of awareness persist. Stigmatization of STIs, including syphilis, can deter individuals from seeking testing and treatment, further fueling transmission rates.
Social determinants of health, including poverty, housing instability, and lack of access to education and employment opportunities, influence syphilis transmission dynamics. These factors create environments conducive to the spread of STIs, including syphilis, and contribute to disparities in infection rates among different population groups.
Stigma and cultural factors also play a significant role in syphilis transmission. Negative attitudes towards sexuality, STIs, and individuals living with syphilis can hinder efforts to prevent and control the spread of the infection. Cultural norms surrounding sexual behaviour, relationships, and healthcare-seeking behaviours can influence individuals’ willingness to engage in preventive measures, including testing and treatment.
Addressing the syphilis epidemic requires a multifaceted approach that addresses the complex interplay of factors contributing to its spread. Efforts to promote sexual health education, increase access to healthcare services, reduce stigma, and address social determinants of health are essential for combating the syphilis epidemic and protecting public health. By addressing these factors comprehensively, healthcare providers, policymakers, and community stakeholders can work together to mitigate the impact of syphilis and improve health outcomes for affected individuals.
Conclusion
In conclusion, this article has provided a comprehensive analysis of the syphilis epidemic in the United States, highlighting key factors contributing to its resurgence and the urgent need for action to address this public health crisis.
Key points discussed include the alarming rise in syphilis cases, reaching levels not seen since the 1950s, and the disproportionate impact on specific demographic groups, including young adults and men who have sex with men. Additionally, the article explored various factors driving the surge in syphilis cases, including changes in sexual behaviour, healthcare access disparities, and challenges in STD prevention and treatment.
The urgency of addressing the syphilis epidemic cannot be overstated. Without concerted efforts to address the underlying factors contributing to its spread, syphilis rates are likely to continue rising, with severe implications for public health.
A call to action is therefore warranted, urging coordinated efforts from healthcare providers, policymakers, and community stakeholders to combat syphilis and reduce its impact on public health. This includes increasing access to sexual health education, testing, and treatment services, as well as addressing social determinants of health and reducing stigma surrounding STIs.
Reference: The U.S. hasn’t seen syphilis numbers this high since 1950. Other STD rates are down or flat